Happy Valentine´s Day to all scientists!
Read more:
The World's Best Photos of clostridium and microbiology
Source: Hivermind
Medical Laboratory and Biomedical Science
Art and Science of Laboratory Medicine. Clinical laboratory and biomedical science related news, abstracts and images for medical laboratory professionals, students and other laboratory geeks.
Art and Science of Laboratory Medicine
Monday, February 13, 2017
Saturday, February 4, 2017
The Pipette
Biomedical Laboratory Science Movie Poster
BMLS - 3B Presents
Source: Facebook via Medtech must know
Image: Anne Caudilla
BMLS - 3B Presents
Source: Facebook via Medtech must know
Image: Anne Caudilla
Friday, February 3, 2017
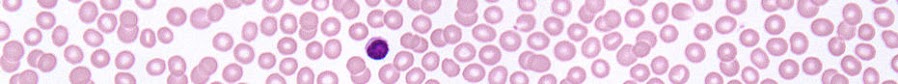
Immature white blood cell fridge magnets
A collection of 5 magnets (~1" round), glass dome magnets. Images depicting immature white blood cells in peripheral blood. band, meta, myelo, promyelo and blast cells
A perfect gift for laboratory friends!
Read more:
Immature white blood cell magnets
Source: WBC by LaboratoryScience via Etsy
A perfect gift for laboratory friends!
Read more:
Immature white blood cell magnets
Source: WBC by LaboratoryScience via Etsy
Sunday, January 29, 2017
Saturday, January 28, 2017
Miss Microbiologist
Miss Universe contestant Chalita Suansane is a 21 year old Thailand native currently studying Microbiology at Mahasarakham University. She is a 3rd year Microbiology student and looks like she still has many things to learn about lab safety...
Read more:
Miss universe
Source: Facebook via Medtech Must Know
Images: (c) KryzzaMelHilay
Read more:
Miss universe
Source: Facebook via Medtech Must Know
Images: (c) KryzzaMelHilay
Sunday, January 22, 2017
Subscribe to:
Posts (Atom)












